CardioNerds Journal Club is a monthly forum for CardioNerds to discuss and breakdown recent publications on twitter and are produced with a corresponding infographic and detailed blog post. For more information, check out the CardioNerds Journal Club Page. This Journal Club focuses on the STRONG-HF Trial.

Table of contents for the ADVOR Trial summary:



September 29, 2022
Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): a multinational, open-label, randomised, trial
Prof Alexandre Mebazaa, MD, Beth Davison, PhD, Prof Ovidiu Chioncel, MD, Prof Alain Cohen-Solal, MD, Rafael Diaz, MD, Prof Gerasimos Filippatos, MD, Prof Marco Metra, MD, Prof Piotr Ponikowski, MD, Prof Karen Sliwa, MD, Prof Adriaan A Voors, MD, Christopher Edwards, BS, Maria Novosadova, MD, Koji Takagi, MD, Prof Albertino Damasceno, MD, Hadiza Saidu, MBBS, Prof Etienne Gayat, MD, Prof Peter S Pang, MD, Prof Jelena Celutkiene, MD, Gad Cotter, MD

Relevant Literature – STRONG-HF Trial
- The first few weeks to months after an acute heart failure hospitalization are a valuable yet vulnerable period for patients.
- While current guidelines recommend early follow-up for patients after discharge for initiation and titration of guideline-directed medical therapy, there is a paucity of data and guidance regarding the timeline and goals for up-titration.

Relevant Guidelines – STRONG-HF Trial
- Relevant Guidelines:
- 2022 AHA/ACC/HFSA Joint Committee Guidelines7: “In patients being discharged after hospitalization for worsening HF, an early follow-up, generally within 7 days of hospital discharge, is reasonable to optimize care and reduce rehospitalization” (Class 2a, LOE B-NR)
- “Multidisciplinary systems of care that promote improved communication between health care professionals, systematic use and monitoring of GDMT, medication reconciliation, and consistent documentation are examples of patient safety standards that should be ensured for all patients with HF transitioning out of the hospital.”
- The 2021 Heart Failure Association of the ESC8 recommends the following:
- 2022 AHA/ACC/HFSA Joint Committee Guidelines7: “In patients being discharged after hospitalization for worsening HF, an early follow-up, generally within 7 days of hospital discharge, is reasonable to optimize care and reduce rehospitalization” (Class 2a, LOE B-NR)

Study Rationale – STRONG-HF Trial
- There is little data behind recommended explicit practices of early follow-up post-discharge for AHF hospitalization. There is a similar lack of data in best practices for optimizing GDMT in the immediate post-discharge period.
Objective – STRONG-HF Trial
To compare high-intensity early follow-up from AHF hospitalization with rapid up-titration of GDMT to target doses within 2-3 weeks of discharge to standard post-discharge care.

Trial9: – STRONG-HF Trial
- Multinational: 14 countries and 87 hospitals
- Open-label trial
- 1:1 parallel-group randomization
Intervention
- Usual care: discharge and follow-up according to local practice for 90 days
- High-intensity care: algorithm-based treatment
- Optimization of oral heart failure therapies:
- First dose adjustment immediately after randomization (within 2 days before anticipated hospital discharge) — prescribed at least half of optimal dose of BB, ACE/ARB/ARNi, and MRA
- Two weeks after randomization, uptitration to full target dose of BB, ACE/ARB/ARNi, and MRA, as tolerated
- Optimization of oral heart failure therapies:
- High-intensity care: algorithm-based treatment

- Frequent visits with circulating NT-proBNP measured
- Assessed by the study team at 1, 2, 3, and 6 weeks after randomization for safety and tolerability by full physical exam and lab assessment of NTproBNP, electrolytes, kidney function, and Hgb
- Diurtics increased based on congestion on physical exam and NT-proBNP
Enrollment Criteria

Outcomes
- Primary Outcome
- 180-day heart failure readmission or all-cause death
- Secondary Outcomes
- Change in quality of life from baseline to day 90 (EQ-5D visual analog scale)
- Change in 180-day all-cause death
- Change in 90-day heart failure readmission or all-cause mortality
- Safety endpoint of incidence of treatment-emergent adverse events up to 90 days
Statistical Analysis
- Intention-to-treat protocol
- Countries combined into regions for analysis, given the sparseness of events in some countries
- Protocol amended to increase sample size and change primary endpoint from 90-day to 180-day mid-way given lower than expected event rate
- The trial terminated when approximately 1000 patients had 90-day follow-up data given larger than expected risk reduction of the primary endpoint in the high-intensity care group

Participant Characteristics:
- The study terminated early due to larger than expected difference in the risk of the primary endpoint between the groups
- The study terminated early due to larger than expected difference in the risk of the primary endpoint between the groups
- N = 1085 (542 to high intensity, 536 to usual care)
- Average age: 63.0 ±13.6
- Male: 662 (61%)
- Race/Ethnicity: 77% white, 21% Black, ≤1% all other
- Average LVEF: 36.3% (±12.52%)
- LVEF ≤40%: 68%
- LVEF >50%: 15% Ischemic cardiomyopathy: 48%
- Ischemic cardiomyopathy: 48%


- Rates of up-titration of meds:
- Percentage of patients on target dose of medication by day 90:
- Reni angiotensin aldosterone inhibition:
- High-intensity group: 55%
- Usual care group: 2%
- Beta-blockers:
- High-intensity group: 49%
- Usual care group: 4%
- Mineralocorticoid receptor antagonist:
- High-intensity group: 84%
- Reni angiotensin aldosterone inhibition:
- Percentage of patients on target dose of medication by day 90:
- Usual care group: 46%

- Average visits in 90 days: 4.8 in high intensity group vs 1.0 in usual care group
- Adjustment treatment effect in vitals and labs:
- Systolic blood pressure (mmHg): -5.4 (-7.2 to –3.5), p < 0.0001
- Diastolic blood pressure (mmHg): -2.3 (-3.5 to –1.1), p = 0.0001
- Pulse (bpm): -5.8 (-7.3 to –4.3), p < 0.0001
- NYHA class: 1.36 (1.22 to 1.53), P < 0.0001
- Bodyweight (kg): -1.36 (-1.91 to –0.80), p < 0.0001
- NT-proBNP (pg/mL): 0.77 (0.67 to 0.89), P = 0.0003
Outcomes



Secondary Outcomes

Adverse Events
- Adverse events in 223/542 patients in the high-intensity group (41%) vs. 158/536 in the usual care group (29%)
- Most commonly observed adverse events: cardiac failure, hypotension, hyperkalemia, renal impairment, with non-significant differences in occurrences between groups
- Hypotension 5% vs. <1%
- Hyperkalemia 3% vs. 0
- Renal impairment 3% vs. <1%
- Bradycardia 0.7% vs. 0.4%

Conclusions
- In this multinational, randomized, open-label trial involving patients discharged following acute heart failure admission, rapid up-titration of guideline-directed medical therapy with scheduled follow-up to achieve specific target doses in the first 90 days was associated with a reduction in 180-day all-cause death or heart failure readmission, improved quality of life, and reduced symptom burden. There was no significant difference in serious adverse outcomes.
Limitations & Considerations
- Early termination of the study given the large treatment effect and concern that it was unethical not to offer high-intensity treatment to both cohorts.
- The composite primary endpoint was not powered to evaluate the difference in 180-day all-cause mortality alone.
- The open-label trial design was necessary based upon intervention, though it may influence the results of self-reported symptom burden as a secondary endpoint.
- SGLTi approval came late in the study and therefore was not prescribed to most patients in the trial.
- Generalizability/feasibility is limited by the availability of resources at individual health centers, though it offers the opportunity to explore the role of telemedicine and the involvement of non-physician care team members in GDMT up-titration.

1. Logeart D, Berthelot E, Bihry N, et al. Early and short-term intensive management after discharge for patients hospitalized with acute heart failure: a randomized study (ECAD-HF). Eur J Heart Fail. Jan 2022;24(1):219-226. doi:10.1002/ejhf.2357
2. Bistola V, Simitsis P, Parissis J, et al. Association between up-titration of medical therapy and total hospitalizations and mortality in patients with recent worsening heart failure across the ejection fraction spectrum. Eur J Heart Fail. Jul 2021;23(7):1170-1181. doi:10.1002/ejhf.2219
3. Yamaguchi T, Kitai T, Miyamoto T, et al. Effect of Optimizing Guideline-Directed Medical Therapy Before Discharge on Mortality and Heart Failure Readmission in Patients Hospitalized With Heart Failure With Reduced Ejection Fraction. Am J Cardiol. Apr 15 2018;121(8):969-974. doi:10.1016/j.amjcard.2018.01.006
4. Carubelli V, Lombardi C, Specchia C, et al. Adherence and optimization of angiotensin converting enzyme inhibitor/angiotensin II receptors blockers and beta-blockers in patients hospitalized for acute heart failure. ESC Heart Fail. Jun 2021;8(3):1944-1953. doi:10.1002/ehf2.13223
5. Gayat E, Arrigo M, Littnerova S, et al. Heart failure oral therapies at discharge are associated with better outcome in acute heart failure: a propensity-score matched study. Eur J Heart Fail. Feb 2018;20(2):345-354. doi:10.1002/ejhf.932
6. Kimmoun A, Takagi K, Gall E, et al. Temporal trends in mortality and readmission after acute heart failure: a systematic review and meta-regression in the past four decades. Eur J Heart Fail. Mar 2021;23(3):420-431. doi:10.1002/ejhf.2103
7. Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e895-e1032. doi:doi:10.1161/CIR.0000000000001063
8. McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. European Heart Journal. 2021;42(36):3599-3726. doi:10.1093/eurheartj/ehab368
9. Mebazaa A, Davison B, Chioncel O, et al. Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): a multinational, open-label, randomised, trial. The Lancet. doi:10.1016/S0140-6736(22)02076-1

The published archive features curated twitter highlights from the journal club event.

SUMMARY:
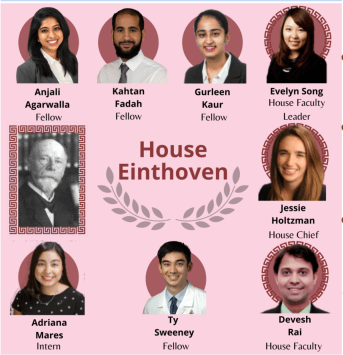
Dr. Anjali Agarwalla, Internal medicine resident, University of Pennsylvania
VISUAL ABSTRACT:
Dr. Ty Sweeney, Internal medicine resident, Johns Hopkins Bayview Medical Center
JOURNAL CLUB PROMO GRAPHIC:
Student doctor Adrianna Mares, medical student, The University of Texas at El Paso
Student doctor Chelsea Amo Tweneboah, medical student, St. George’s University,
TWEET PREPARATION:
Dr. Gurleen Kaur, Internal medicine resident, Brigham Women’s Hospital
Dr. Kahtan Fadah, Internal medicine resident, Texas Tech University
HOUSE JONES CHIEF FELLOW:
Dr. Jessie Holtzman, Chief resident, UCSF
HOUSE JONES FACULTY
Dr. Devesh Rai, @DeveshRaiMD, Cardiology fellow at Rochester General Hospital
DIRECTOR of JOURNAL CLUB:
Dr. Devesh Rai, @DeveshRaiMD, Cardiology fellow at Rochester General Hospital