Podcast: Embed
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | Pandora | iHeartRadio | Blubrry | TuneIn | Deezer | RSS
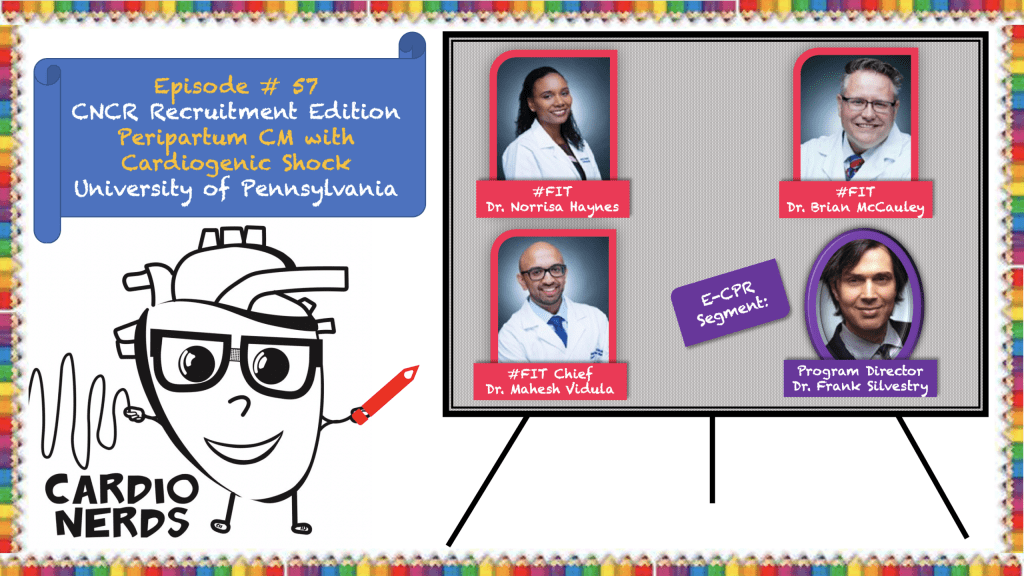
CardioNerds (Amit Goyal & Daniel Ambinder) join Penn cardiology fellows (Brian McCauley, Norrisa Haynes, and Mahesh Vidula) for a rooftop picnic in sunny Philadelphia! They discuss an informative case of peripartum cardiomyopathy with cardiogenic shock. Program director Dr. Frank Silvestry provides the E-CPR segment and a message to applicants. Johns Hopkins internal medicine resident Colin Blumenthal with mentorship from University of Maryland cardiology fellow Karan Desai.
Jump to: Patient summary – Case figures & media – Case teaching – References – Production team
The CardioNerds Cardiology Case Reports series shines light on the hidden curriculum of medical storytelling. We learn together while discussing fascinating cases in this fun, engaging, and educational format. Each episode ends with an “Expert CardioNerd Perspectives & Review” (E-CPR) for a nuanced teaching from a content expert. We truly believe that hearing about a patient is the singular theme that unifies everyone at every level, from the student to the professor emeritus.
We are teaming up with the ACC FIT Section to use the #CNCR episodes to showcase CV education across the country in the era of virtual recruitment. As part of the recruitment series, each episode features fellows from a given program discussing and teaching about an interesting case as well as sharing what makes their hearts flutter about their fellowship training. The case discussion is followed by both an E-CPR segment and a message from the program director.
CardioNerds Case Reports Page
CardioNerds Episode Page
CardioNerds Academy
Subscribe to our newsletter- The Heartbeat
Support our educational mission by becoming a Patron!
Cardiology Programs Twitter Group created by Dr. Nosheen Reza

Patient Summary
Two weeks postpartum, a woman in her mid 20s, G1P1, with no past medical history presented following a tonic-clonic seizure. Prior to this, she had been experiencing 1 week of worsening dyspnea and lower extremity edema. Initial work-up revealed a left MCA stroke and she underwent thrombectomy. Limited TTE found LVEF <20% and a LV apical thrombus; she was started on milrinone due to concern for cardiogenic shock and transferred to the University of Pennsylvania.
Upon arrival, she was found to be hypotensive and tachycardic. Exam was notable for elevated JVP, +S3, LE edema and R sided hemiparesis. Labs showed multiorgan injury, elevated NT-proBNP and elevated lactate. EKG demonstrated sinus tachycardia with no ST-T changes. Formal TTE showed severely dilated LV with EF 10%, diffuse LV hypokinesis, and confirmed a large LV apical thrombus. A pulmonary artery catheter was placed for tailored therapy and found elevated L-sided > R-side filling pressures with low cardiac index despite inotropes. Cardiac power output (CPO) was severely decreased with borderline pulmonary artery pulsatility index (PAPI), corroborating left > right heart failure. Patient ultimately required a durable left ventricular assist device (LVAD). Over the course of 9 months her guideline directed medical therapy (GDMT) was titrated and her intrinsic cardiac function and symptoms improved. Her EF improved to 35-40% and she tolerated an LVAD weaning protocol, so her LVAD was ultimately explanted! She is currently doing well on GDMT alone!
Episode Schematics & Teaching
The CardioNerds 5! – 5 major takeaways from the #CNCR case
1. How do we define Peripartum Cardiomyopathy?
- Diagnosis is made by the development of heart failure towards the end of pregnancy or in the months following delivery (~5 months postpartum), no other identifiable cause of HF, and demonstration of LV systolic dysfunction with LVEF typically less than 45% with or without dilation.
- Risk factors include history of pre-eclampsia, hypertension, cocaine use, multifetal pregnancies, older maternal age, and African descent.
- Keep a broad differential diagnosis for new onset heart failure in the peripartum period. The differential includes pre-existing cardiomyopathy, valvular disease or congenital cardiomyopathy unmasked by the hemodynamic changes of pregnancy (see CNCR episode 48 for more on the hemodynamic changes of pregnancy!). Other differentials should include ischemia/spontaneous coronary artery dissection (SCAD), stress-induced cardiomyopathy, CM due to systemic disease (e.g. sepsis, rheumatologic disease), myocarditis and tachycardia-induced CM.
2. The team used invasive hemodynamics to guide shock management. Why is a PAC helpful?
- Despite data from the ESCAPE trial, a pulmonary artery catheter (PAC) can be very useful in the diagnosis and management of cardiogenic shock. Remember, the ESCAPE trial included chronic HF patients in whom there was clinical uncertainty on whether a PAC may be useful. Further, any patient on milrinone was excluded. Cardiac power output (CPO) and pulmonary artery pulsatility index (PAPi) are some of the parameters obtained from a PAC that can guide cardiogenic shock therapy and need for mechanical circulatory support (MCS).
- Resting CPO = CO x MAP / 451. CPO measures the “pumping power” of the LV and correlates with end-organ perfusion. In the SHOCK registry, CPO <0.53 watts highly correlated with ↑ in-hospital mortality. CPO can also help identify patients ready for LVAD weaning trials and/or explantation. As with most cardiac parameters, the trends matter as much as the absolute values!
- PAPi: PA(Systolic) – PA(diastolic) / RA(mean). PAPi was initially developed as a marker severe RV dysfunction in acute inferior wall myocardial infarction and those undergoing LVAD placement. It measures the ratio of the PA pulse pressure to a given preload (RA pressure). It is hard to apply PAPi thresholds across different clinical situations, but we can generally use less than 1-1.75 as a predictor of worsening right-sided function.
3. How should we approach “typical HF” management in peripartum cardiomyopathy?
- Though many aspects of the acute management of peripartum cardiomyopathy are similar to typical heart failure and/or cardiogenic shock management, there are a few key differences.
- Remember, ACEI/ARBs/ARNI and spironolactone are contraindicated during pregnancy. ACE-I have demonstrated safety data while breastfeeding, but ARNIs and ARBs have not been studied robustly.
- The decision to pursue an ICD in patients with PPCM needs special attention to the natural history of PPCM. Many of these patients will have recovery of LV function in 3-12 months, thus deferring primary prevention ICD while titrating GDMT for ~6 months may be appropriate. There may also be a role for a wearable cardioverter/defibrillators in those with severe LV dysfunction as a bridge to recovery or until an implantable ICD is indicated.
- Consider early mechanical support in patients deteriorating on medical therapy (including inotropes) alone.
4. What are some considerations unique to peripartum cardiomyopathy management?
- The prothrombotic state of pregnancy and stasis within a weak ventricle both increase the risk of LV thrombus and a subsequent cardio-embolic event. Therefore, anticoagulation should be considered in PPCM patients with a severely reduced LVEF (EF < 30% by AHA vs ≤35% by ESC) during late pregnancy and 6 to 8 weeks postpartum. LMWH does not cross the placenta and is preferred during pregnancy. Both warfarin and LMWH may be used during lactation, while the direct oral anticoagulants have not been studied either during pregnancy or lactation and should be avoided.
- Bromocriptine, a dopamine agonist, reduces prolactin levels (a possible culprit in the development of PPCM). However, data is conflicting on benefit, and thus this therapy should be considered investigative. It is pro-thrombotic, and so it is recommended for patients to be on anticoagulation if bromocriptine is used.
- Prior to delivery, multidisciplinary discussions should occur around timing and method of delivery for patients diagnosed with PPCM during pregnancy. During delivery, remember that there are several hemodynamic changes (See Ep #48 – AS Complicating Pregnancy!). These include increased preload from placental auto-transfusion and relief of IVC compression.
- The 2018 ESC guidelines suggest avoiding breastfeeding in patients with severe HF because of the high metabolic demands of lactation and the induced prolactin may contribute to worsening HF. However, some small studies suggest in clinically stable patients, breastfeeding does not worsen HF symptoms or LVEF. Considerations regarding possible risk must be counterbalanced with the known benefits of breastfeeding for infants and mothers.
5. How do we approach long-term management in patients with peripartum cardiomyopathy?
- Providers should engage in shared decision-making about future pregnancies in patients with recovered EF (>50%) as they are at higher risk of future recurrence. The 2018 ESC guidelines advise against pregnancy if EF has not recovered to >50-55%.
- Contraception counseling should be done early: before discharge or at the time of diagnosis. Patients should avoid estrogen-containing methods especially in the early postpartum period as thromboembolism risk is high.
- If a patient plans on another pregnancy, teratogenic HF medications, like ACE/ARB/ARNI and spironolactone, must be stopped prior to stopping contraception. Following cessation of these GDMT medication, follow-up echocardiography to ensure LV functional stability should be performed after at least 3 months off therapy. The patient should be monitored very closely during a subsequent pregnancy for changes in symptoms and followed with serial echocardiograms and NT-proBNP levels during pregnancy and thereafter.
References
- Davis MB, Arany Z, McNamara DM et al. Peripartum Cardiomyopathy: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75(2):207-221. doi:10.1016/j.jacc.2019.11.014
- Korabathina R, Heffernan KS, Paruchuri V, et al. The pulmonary artery pulsatility index identifies severe right ventricular dysfunction in acute inferior myocardial infarction. Catheter Cardiovasc Interv. 2012;80(4):593-600. doi:10.1002/ccd.23309
- Kang G, Ha R, Banerjee D. Pulmonary artery pulsatility index predicts right ventricular failure after left ventricular assist device implantation [published correction appears in J Heart Lung Transplant. 2017 Nov;36(11):1272]. J Heart Lung Transplant. 2016;35(1):67-73. doi:10.1016/j.healun.2015.06.009
- Kochav SM, Flores RJ, Truby LK, Topkara VK. Prognostic Impact of Pulmonary Artery Pulsatility Index (PAPi) in Patients With Advanced Heart Failure: Insights From the ESCAPE Trial. J Card Fail. 2018;24(7):453-459. doi:10.1016/j.cardfail.2018.03.008
- Lim HS, Gustafsson F. Pulmonary artery pulsatility index: physiological basis and clinical application. Eur J Heart Fail. 2020;22(1):32-38. doi:10.1002/ejhf.1679
- Fincke R, Hochman JS, Lowe AM, et al. Cardiac power is the strongest hemodynamic correlate of mortality in cardiogenic shock: a report from the SHOCK trial registry. J Am Coll Cardiol. 2004;44(2):340-348. doi:10.1016/j.jacc.2004.03.060
- Mendoza DD, Cooper HA, Panza JA. Cardiac power output predicts mortality across a broad spectrum of patients with acute cardiac disease. Am Heart J. 2007;153(3):366-370. doi:10.1016/j.ahj.2006.11.014

















